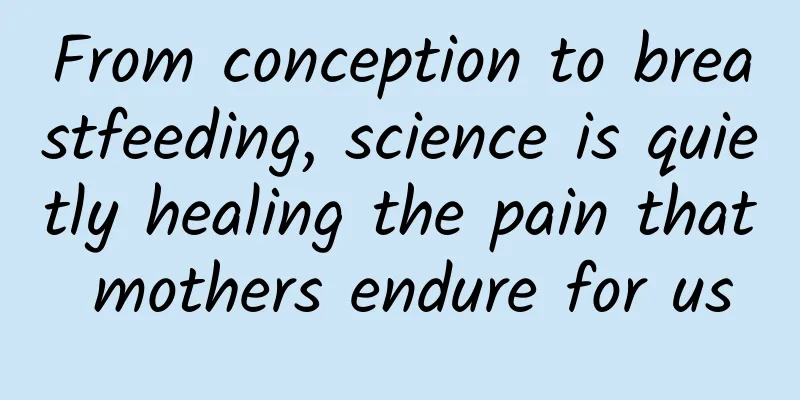
From conception to breastfeeding, science is quietly healing the pain that mothers endure for us
|
Mothers give us life. It is not until we grow up, or even grow old, that we gradually realize what that means. In the time of creating new life, all the pain that mothers are forced to endure should be seen, acknowledged, and changed. Written by | Xiaoye Throughout the ages, people have generously dedicated the most beautiful eulogies to mothers, but the long-lasting pain that women endure from pregnancy to postpartum breastfeeding cannot be expressed in words. It is science that silently supports mothers all over the world and tries its best to alleviate the pain they have to endure. Conception: Blessings and unspeakable pain Most pregnant women cannot escape the discomfort of pregnancy, many of which are pain. As hormone levels change and the fetus continues to grow, there is always a pain from head to toe that may target pregnant women: headaches, shoulder pain, breast swelling, cracking and stinging, burning pain in the stomach, back pain, pelvic pain, leg muscle stiffness and pain, swelling and pain in the extremities... These are all common pains during pregnancy [1, 2]. Everyone has a different physique, and the severity of pregnancy pain varies from person to person. So far, epidemiological studies on pain during pregnancy are still scarce, but existing results still show that back pain and pelvic pain are the most likely to affect the normal life of pregnant women, often causing them to seek medical attention due to the pain. According to three studies from Nepal (2019), Norway (2012) and Sweden (2005) [3-5], the prevalence of low back pain and/or pelvic pain associated with pregnancy ranges from 34% to 72%. In Nepal, 1,284 pregnant women participating in the survey reported that their low back and pelvic pain was an average of level 6 (Figure 1), which is "unbearable and obvious moderate pain, sleep disturbance, and the need for analgesia". Figure 1. Pain is measured using the Numerical Rating System (NRS), where 0 means “no pain at all” and 10 means “the most severe pain.” Level 4 pain affects sleep, and level 7 pain prevents sleep. [10] Nowadays, more and more pregnant women no longer choose to endure in silence and ask doctors to prescribe painkillers. Common analgesics include non-steroidal anti-inflammatory drugs (such as ibuprofen), acetaminophen (also known as acetaminophen, paracetamol) and opioids. Unfortunately, they all have an impact on fetal development. The FDA (U.S. Food and Drug Administration) does not recommend that women who are pregnant for more than 20 weeks take non-steroidal anti-inflammatory drugs because they may cause the baby to suffer from serious rare liver diseases before birth [7]. A 2021 review pointed out that acetaminophen may interfere with the development of the fetus's brain, reproductive and urinary systems, bringing negative effects [8, 9]. In Europe and the United States, more and more pregnant women are using opioids for pain relief. A cohort study by a team from the University of Montreal in Canada found that the prevalence of opioid use during pregnancy increased by 40.3% from 1998 to 2005. Specifically, the number of women using drugs during the two periods of gestation, 16-28 weeks of pregnancy and 28 weeks of pregnancy until delivery, increased significantly [10]. In the United States, from 2010 to 2017, the number of mothers with opioid-related diagnoses during pregnancy increased by 131%, while the number of babies born with neonatal abstinence syndrome increased by 82% [11, 12]. A self-report in 2019 showed that 6.6% of the women surveyed (a total of 20,643 people) admitted to taking prescription opioids during pregnancy. [13] Therefore, although the number of pregnant women taking painkillers is increasing, given that the drugs may have adverse effects on the mother and fetus, expectant mothers must strictly follow the doctor's advice, maintain a safe dosage, and protect the health of themselves and their babies. Figure 2. A pregnant woman with back pain. Source: unsplash Childbirth: Pain relief technology brings hope After ten months of pregnancy, once the baby is born, pregnant women will face the peak challenge of physical pain. Using the numerical rating method, from the beginning of the initial contraction, the continuous pain can reach level 2-3, and the most severe contraction can reach level 7-8 [14]. However, simple numbers cannot make people truly empathize with the pain. Each mother's description is different: "It rises and falls like the tide, then recedes and rises again", "The body is crushed and the bones are about to be pulled apart", "It feels like someone is hammering my stomach and waist with a hammer and stabbing me with a knife", "It's like my waist is broken, and the scary thing is that it will repeat itself a few minutes later..." [15] When there is pain, it is natural to find ways to relieve it. In the history of both the East and the West, there are records of the use of opium and folk herbs to relieve labor pain, as well as various folk remedies such as olive oil massage and taking eel gallbladders[16]. However, under the guidance of strong traditional concepts and religious beliefs, enduring labor pain has always been regarded as a natural responsibility of women, and relieving the pain of mothers has never been the primary task in the delivery process. For thousands of years, women have silently endured the pain of natural childbirth. But medicine did not abandon suffering women. Soon after the birth of modern anesthesia, labor analgesia was brought to the fore. In 1846, American dentist William Morton successfully demonstrated the effects of inhaled ether anesthesia at the Massachusetts General Hospital affiliated with Harvard University, creating a new era of surgery. A year later, another American dentist, Dr. Nathan Cooley Keep, published an article in the Boston Medical Surgical Journal[17], reporting that he had successfully relieved labor pain by using ether gas while assisting a woman in natural childbirth. The first woman in the world to receive labor analgesia was named Fanny Appleton Longfellow, the second wife of the famous American poet Henry Wadsworth Longfellow. With the help of Keep, she successfully gave birth to her third child[18]. Figure 3. (Left) Nathan Cooley Keep (1800-1875)[19]; (Right) Keep’s patient, Fanny Longfellow (1817-1861), the first woman in the world to successfully receive ether analgesia during childbirth[20] At the same time, on the other side of the Atlantic Ocean, James Simpson, a professor of midwifery at the University of Edinburgh in the United Kingdom, also used ether as an anesthetic for the first time to help a pregnant woman deliver a dead baby that had failed to invert itself.[21] He then began to look for other anesthetics with similar functions to ether, and soon discovered chloroform with his colleagues, which he successfully helped a woman deliver a baby two weeks early: he soaked a teaspoon of chloroform in a handkerchief rolled into a funnel, and then placed it upside down over the mouth and nose of the woman. According to his own record, "the woman delivered the baby successfully within 25 minutes after inhaling the chloroform."[22] Of course, the most famous case of chloroform analgesia during labor was when Queen Victoria (1819-1901) of the United Kingdom gave birth to Prince Leopold in 1853. The queen remained conscious during the delivery, but did not feel any pain. As a boon for mothers, labor analgesia quickly became popular. In 1848, the American Medical Association reported 2,000 cases of anesthetic use during childbirth, and the number of complications was small and not serious. Despite this, opposition still existed, on the one hand from biblical doctrine, and on the other hand from within the medical community - many people believed that the pain of mothers during childbirth was a meaningful clinical indication, and eliminating pain might inhibit childbirth and sever the emotional bond between mother and baby. In response, Simpson and his colleagues insisted on defending the necessity of labor analgesia and promoting the positive significance of anesthetics. With the Queen's endorsement, by 1862, obstetric anesthesia had become quite common, but doctors in different places had their own preferences for the choice of anesthetics [16]. Figure 4. (Left) James Simpson (1811-1870) (Right) Queen Victoria (1819-1901) had 9 children in her lifetime, and Prince Leopold was her eighth child. In addition to ether and chloroform, nitrous oxide, discovered in the 18th century It has also been increasingly used for labor analgesia since the beginning of the 20th century. Different doctors have also tried to mix nitrous oxide with oxygen in an effort to overcome the problem that nitrous oxide can cause hypoxia. The method of using nitrous oxide to relieve labor pain has been used to this day [16]. In parallel with the inhalation analgesia method, there are two other different techniques. The first is called the "parenteral technique", which became a routine operation for midwives in the 1920s. However, the process is relatively cumbersome: when the mother's cervix dilates to 2-3 cm, or the pain of uterine contractions becomes regular and the interval is 5 minutes, the midwife will first perform a continuous enema, and then inject morphine and magnesium sulfate at a specific dose at a certain interval. Then the mother is helped to lie down, the perineum is cleaned, and vaseline is applied to the rectal area to relieve irritation. Then a gastrointestinal catheter is inserted, and an olive oil-ether mixture is slowly dripped in over the next 30 to 60 minutes. The use of parenteral technology can effectively relieve pain without affecting the delivery process. However, this method also has disadvantages: pregnant women are prone to fall asleep due to the effects of drugs during delivery, so midwives need to remain vigilant throughout the process. Secondly, this technique can easily anesthetize the fetus and irritate the rectum. Sometimes forceps may be needed to pull the baby out [23]. The second method is a local anesthesia method. In 1921, Spanish military doctor and surgeon Fidel Pages reported epidural anesthesia, which uses a catheter to inject anesthetic drugs into the epidural space of the waist. The drugs block the transmission of signals from nearby spinal nerves, thereby temporarily making people lose their sense of pain. More than 20 years later, American anesthesiologist John Bonica began to promote the use of epidural anesthesia during childbirth. His wife had life-threatening complications from ether analgesia during the birth of her first child. Therefore, when giving birth to her second child, Bonica used epidural anesthesia to relieve his wife's pain. His wife thus became the first woman in the world to successfully receive epidural anesthesia. By the 1970s and 1980s, epidural anesthesia for labor analgesia had become popular throughout the United States. According to statistics, between 1981 and 1997, the proportion of labor analgesia in major hospitals across the United States was close to 70% [24]. Figure 5. (Left) Fidel Pagés (1886-1923); (Right) John J. Bonica (1917 – 1994)[25] The labor analgesia techniques mentioned above all use anesthetics or sedatives, but there are always women who cannot use these drugs or who are worried that the drugs may have adverse effects on the mother and baby. Therefore, non-drug labor analgesia methods can also be selected in obstetric practice. For example, in recent decades, water birth has become popular in European countries. This method can be traced back to 1805, when a French woman suffered several hours of labor pains. Her doctor decided to let her lie in a bathtub filled with hot water. As a result, the child was born soon and both mother and child were safe [26]. The first medical report of a baby born in water was that of American Jeremy Lighthouse, who was born in a warm bathtub in 1980. In the 1970s, water birth became widely spread and popular. After observing nearly a thousand cases of water birth, doctors found that women who gave birth did prefer the water environment. They felt mentally relaxed, physically comfortable, pain relieved, and could control the birth process independently. [27] By 1993, all maternity centers in England and Wales were equipped with water birth equipment to help more women achieve water births. The UK National Health Service also included water birth in labor analgesia methods and provided detailed guidance [28, 29]. In sharp contrast to the UK's enthusiasm, the United States has a cautious attitude. In 2014, the American College of Obstetricians and Gynecologists published an article on its official website stating [26] that there is currently insufficient data to clarify the benefits and risks of water births for women in the second stage of labor. Therefore, water births should still be considered an experimental method and should be conducted in trials and monitored. Labor analgesia technology has been developed in Europe and the United States for more than 150 years and is now quite mature. It helps women solve the biggest difficulty they face during childbirth and makes them no longer particularly afraid of childbirth. According to statistics, the labor analgesia rate in developed Western countries has reached 85-98%, which fully demonstrates that receiving analgesia during natural childbirth has become a normal and widely accepted concept. China’s painless childbirth research started not too late. As early as 1963, Professor Zhang Guangbo, an obstetrician and gynecologist at Peking University Hospital and the first person in China to perform painless childbirth, used low-concentration procaine to provide labor analgesia for 67 women in labor, and recorded 50 clinical samples in detail. He then presented a paper titled “Continuous Epidural Block for Painless Childbirth” at the First National Anesthesia Academic Conference held in Nanjing, confirming the feasibility of painless childbirth[17]. Figure 6. (Left) The original version of Zhang Guangbo’s paper. Photo by Zhang Lingyun[30]; (Right) Zhang Guangbo, the first person in China to perform painless childbirth[31] Unfortunately, Zhang Guangbo's research was stranded in the tide of history. Fortunately, we are catching up. In the 1990s, Yao Shanglong, an anesthesiologist at Wuhan Union Hospital, went abroad to attend the annual meeting of the American Society of Anesthesiologists (ASA) and was exposed to labor analgesia technology. After returning to China, he actively carried out clinical trials and published articles. In 2000, Nanjing Maternal and Child Health Hospital tried to promote labor analgesia; in August 2001, Peking University Hospital carried out labor analgesia on a large scale, and started training courses in February of the following year to promote labor analgesia technology nationwide. In 2008, Hu Lingqun, an associate professor of anesthesiology at Northwestern University Feinberg School of Medicine, launched the "Painless Childbirth China Tour", leading nearly a thousand American medical staff to cooperate with more than 100 hospitals in China to promote labor analgesia. In the same year, Xu Mingjun, a professor of anesthesiology at Beijing Obstetrics and Gynecology Hospital, also launched the "Kangle Labor Analgesia National Promotion Project". In 2018, the National Health Commission issued the "Labor Analgesia Pilot Work Plan". In 2022, the National Health Commission's assessment showed that the rate of intrathecal labor analgesia in 912 pilot hospitals across the country increased from 27.52% in 2017 to 53.21% in 2020[32]. However, the overall rate of labor analgesia in my country is currently only about 30%, and there is still a long way to go before more Chinese women can benefit from labor analgesia. Postpartum: Where is the end of the pain journey? After all the hard work of giving birth, the pain in the body does not disappear immediately. The type, intensity, and duration of postpartum pain vary from person to person. Clinically, the more common symptoms include uterine cramps, neck, back, or joint pain, perineum swelling and pain, postoperative wound pain, breast swelling, urination pain, hemorrhoids, etc. [33] In addition to physical pain, hormonal changes in the body after childbirth make women's mood swings more intense, which can easily cause mental "pain" - postpartum depression. (This article will not go into detail here.) However, in general, as the body recovers after childbirth, the pain will gradually subside, which may take a few days or even half a year. In the past decade, more and more women have reported persistent pain after childbirth, which has attracted the attention of the government, medical institutions and the public. A meta-study published in the European Journal of Anaesthesiology in 2016 showed that 11% of women who underwent caesarean section experienced persistent pain for up to 12 months after delivery[34]. In 2020, a team from the University of Washington in the United States revealed factors associated with persistent postpartum pain (more than 6 months) [35]: the first is the mode of delivery, for example, cesarean section may leave scar pain; secondly, persistent vaginal and perineal pain is related to surgical vaginal delivery and the degree of perineal trauma; finally, a history of back pain before and during pregnancy and overweight are also associated with persistent back pain after delivery. In addition to the pain that is difficult to dissipate after childbirth, breastfeeding is also an absolutely unpleasant experience. The pain caused by breastfeeding is devastating. During breastfeeding, the breasts become engorged with blood and become hard, tight, and heavy. The milk must be drained as quickly as possible. The frequent sucking (and sometimes biting) of the mother’s nipples by the baby can cause nipple blood vessel spasms or nipple rupture, resulting in open wounds. Many mothers also face blocked milk ducts and soreness, tenderness, and burning pain caused by mastitis. In order to empty their breasts and heal as quickly as possible, mothers have to continue breastfeeding despite the pain of inflammation.[36] Some even say that breastfeeding is more painful than giving birth. Figure 7. A peaceful and wonderful breastfeeding experience is not so easy to obtain. 丨Source: unsplash In 2021, a study published in the International Breastfeeding Journal investigated the pain perception of breastfeeding women[37] and directly recorded the voices of many mothers: "My nipples were cracked, bleeding and blisters formed. I could only bite the towel and stamp my feet, but I still screamed in pain." "Both my nipples cracked and I had to keep putting moisturiser on them. One is still sore but it seems to be healing." Some breastfeeding women often feel that their chests have been "suddenly hit", and this is not limited to the breasts, but also includes the chest area including the shoulders: "I have been breastfeeding for 8 months, and suddenly one day, my chest seemed to be punched hard, and it hurt like hell." In fact, with the development of obstetrics, there is a mature and complete set of postpartum care operations to help relieve women's pain after childbirth. There are various non-drug care methods for different types and locations of pain, such as ice compresses, heating pads, breast protectors, medical abdominal belts, etc., which can produce a certain analgesic effect [38, 39]. In addition, different countries also provide their own lists of medicines and dosage instructions for reference by postpartum and lactating women. For example, the National Health Service in the United Kingdom recommends that mothers take different types of analgesics according to the degree of pain [40]. Similarly, the American College of Obstetricians and Gynecologists has proposed a multimodal analgesia approach of nonsteroidal anti-inflammatory drugs, acetaminophen, and mild opioids, and especially recommends the combined use of nonsteroidal anti-inflammatory drugs and acetaminophen. Strong opioid analgesics should only be considered when the previous drugs have been fully used and are ineffective [41, 42]. It is worth noting that in any country, the use of opioids by pregnant women or postpartum women is strictly controlled, because taking opioids in the early postpartum period can cause constipation and aggravate perineal pain; and the drowsiness of the mother after taking the drug will also affect her daily care and feeding of the baby. In addition, opioids are often lipophilic, low molecular weight, and weakly alkaline, which help the drug ingredients penetrate into breast milk. As early as 2007, a study from Australia pointed out that oxycodone will accumulate in breast milk within 72 hours after delivery. Although low-dose short-term use does not require stopping breastfeeding, it still needs to be closely observed [43]. Another study in the same year investigated another opioid, codeine [44]. After taking codeine, the human body will produce more morphine. If taken for a long time, the newborn will face a higher risk of morphine poisoning. Therefore, the research team recommends that doctors avoid prescribing codeine to mothers as much as possible. If there is no other choice, it is recommended that the drug be taken for only 2 to 3 days. However, a study published in the journal Clinical Toxicology in 2011 showed that short-term use of opioids prescribed by doctors by breastfeeding mothers is often safe and rarely endangers the health of newborns [45]. On March 15 this year, The BMJ (British Medical Journal) published the world's largest survey on the effects of maternal opioid use on newborns [46]. A total of 865,691 mother-infant pairs in Canada participated in this study over a period of nearly 8 years. The results showed that mothers taking opioids as prescribed after childbirth did not increase the risk of their babies being re-hospitalized shortly after birth, nor did they increase the rate of adverse reactions to their babies, nor did they cause infant deaths. Therefore, the investigators support the cautious use of short-term postpartum opioids by breastfeeding mothers.
References 1 https://m.medsci.cn/article/show_article.do?id=86a2159061fc 2 https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/ 3 https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-019-2398-0#:~:text=The%20prevalence%20of%20pregnancy%2Drelated,8%2C9%2C10%5D. 4 https://www.jmptonline.org/article/S0161-4754(12)00058-9/fulltext 5 https://journals.lww.com/spinejournal/Abstract/2005/04150/Low_Back_Pain_and_Pelvic_Pain_During_Pregnancy_.22.aspx 6 https://www.physio-pedia.com/Numeric_Pain_Rating_Scale 7 https://www.fda.gov/drugs/drug-safety-and-availability/fda-recommends-avoiding-use-nsaids-pregnancy-20-weeks-or-later-bec ause-they-can-result-low-amniotic#:~:text=FDA%20is%20warning%20that%20use,some%20cases%2C%20neonatal%20renal%20impairment. 8 https://www.nature.com/articles/s41574-021-00553-7 9 https://www.health.harvard.edu/blog/is-a-common-pain-reliever-safe-during-pregnancy-202110292627 10 https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-021-04270-x 11 https://www.cdc.gov/pregnancy/opioids/articles.html 12 https://jamanetwork.com/journals/jama/fullarticle/2774834 13 https://www.cdc.gov/mmwr/volumes/69/wr/mm6928a1.htm 14 https://www.medsci.cn/article/show_article.do?id=1865151600c4 15 https://www.nfpeople.com/article/10492 16 https://journals.sagepub.com/doi/pdf/10.1177/0310057X150430S106 17 Keep, NC (1847b). Letters & medical intelligence. Boston Medical and Surgical Journal, 36, 226 18 https://en.wikipedia.org/wiki/Nathan_Cooley_Keep 19 https://doi.org/10.1016/j.joms.2011.02.121. 20 https://www.nps.gov/long/learn/historyculture/fanny-longfellow.htm 21 https://www.haodf.com/neirong/wenzhang/27602.html 22 https://fn.bmj.com/content/86/3/F207 23 https://www.jognn.org/article/S0884-2175(17)30036-9/pdf 24 http://www.xinhuanet.com/politics/2018-10/12/c_1123547877.htm 25 https://www.iasp-pain.org/person/in-memoriam-john-j-bonica/ 26 https://www.nytimes.com/2020/04/15/parenting/pregnancy/water-birth.html 27 https://onlinelibrary.wiley.com/doi/full/10.1111/1751-486X.12144 28 https://www.nhs.uk/pregnancy/labour-and-birth/what-happens/pain-relief-in-labour/ 29 https://www.nct.org.uk/labour-birth/different-types-birth/water-birth/how-labour-water-or-have-water-birth 30 https://www.shobserver.com/wx/detail.do?id=93352 31 https://www.sohu.com/a/585247251_100042026 32 http://www.nhc.gov.cn/yzygj/ylyxjg/202208/f4dcfe85933040558fe69ebc345a55a1.shtml 33 https://www.acog.org/womens-health/faqs/postpartum-pain-management 34 https://journals.lww.com/ejanaesthesiology/Fulltext/2016/11000/Incidence_and_severity_of_chronic_pain_after.9.aspx 35 https://www.bjanaesthesia.org.uk/article/S0007-0912(20)30002-7/fulltext#%20 36 https://www.mamava.com/mamava-blog/fast-fixes-common-breastfeeding-problems 37 https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-021-00426-9 38 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5962320/ 39 https://linkinghub.elsevier.com/retrieve/pii/S1751485121002531 40 https://www.royalberkshire.nhs.uk/media/czjctilg/pain-relief-after-birth_july21.pdf 41 https://www.acog.org/clinical/clinical-guidance/clinical-consensus/articles/2021/09/pharmacologic-stepwise-multimodal-approach-for-postpartum-pain-management 42 https://www.haodf.com/neirong/wenzhang/8963519343.html 43 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1952551/ 44 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1952551/ 45 https://www.tandfonline.com/doi/full/10.3109/15563650.2011.635147#:~:text=The%20short%2Dterm%20maternal%20use,a%20hazard%20to%20the%20newborn. 46 https://www.bmj.com/content/380/bmj-2022-074005 47 https://www.statnews.com/2019/07/26/persistent-opioid-use-after-childbirth/ 48 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2739048 This article is supported by the Science Popularization China Starry Sky Project Produced by: China Association for Science and Technology Department of Science Popularization Producer: China Science and Technology Press Co., Ltd., Beijing Zhongke Xinghe Culture Media Co., Ltd. Special Tips 1. Go to the "Featured Column" at the bottom of the menu of the "Fanpu" WeChat public account to read a series of popular science articles on different topics. 2. Fanpu provides a function to search articles by month. Follow the official account and reply with the four-digit year + month, such as "1903", to get the article index for March 2019, and so on. Copyright statement: Personal forwarding is welcome. Any form of media or organization is not allowed to reprint or excerpt without authorization. For reprint authorization, please contact the backstage of the "Fanpu" WeChat public account. |
>>: Do “sleep-aiding foods” really help you sleep?
Recommend
Ideal Auto: In August 2022, Ideal Auto delivered a total of 4,571 vehicles, two-thirds lower than its peak period
Ideal Auto released its sales results for August,...
Chen Jiangxiong-Douyin Follower Increase and Traffic Training Camp
Chen Jiangxiong's Douyin fan increase and tra...
Ministry of Industry and Information Technology: Pop-up ads are strictly prohibited in elderly-friendly apps, and websites must provide extra-large fonts
IT Home reported on April 7 that in order to carr...
Want to become a high-level SEM promotion and marketing expert? You must go through these 5 stages
The author divides bidders into 5 levels: 1. Novi...
Pinduoduo goes all in on the real economy, and big data empowers the rise of domestic products
Once upon a time, when people mentioned "dom...
Brilliance is panicking. BMW plans to increase its stake in the joint venture to 75% and transform it into a global production base.
According to German Manager Magazine, BMW's s...
New changes in marketing in 2022
The first wave of marketing boom in 2022 was born...
China Automotive Power Battery Industry Innovation Alliance: Ranking of domestic power battery manufacturers in January 2022
Recently, the China Automotive Power Battery Indu...
Ten thousand words of useful information! Core user acquisition and operation strategies (including Xiaohongshu and Zaixing cases)
Introduction: This article is the second 10,000-w...
In some places in Hainan, this tree is more famous than the coconut tree →
Walking in Hainan, you can see coconut trees ever...
Case analysis: Explosive growth of operational activities!
User Growth (UG for short), like the concept of “...
Interpretation of iResearch's 2014 DSP Industry Analysis Report
iResearch recently released the "2014 DSP In...
Li Bingjun's resume: The key points of on-site SEO promotion
On-site SEO promotion focuses on on-site SEO opti...
Lazy Field · Today's Toutiao project gameplay, Toutiao video project, single number income is 50-500 can be batched
Lazyman Field·How to play the Toutiao project, a v...
6 analysis methods to teach you how to quickly diagnose SEM account performance
Only data can tell whether your promotion account...